As guided surgery continues to grow in the dental industry, it is becoming common knowledge that a CBCT and diagnostic cast are the basic requirements to have a 3D fabricated surgical guide created.
However, digital dentistry demands digital files and today's technology has provided numerous ways to acquire that. But how is a clinician to decide which route to take? Should the clinician take a traditional impression or invest in an intraoral scanner? If the clinician does choose to take a traditional impression, should he/she then invest in an optical scanner? Or try to utilize model scanning features that many CBCT units are starting to offer? To identify the pros and cons of each option, one first needs to understand the role a diagnostic cast plays in surgical guide design and the nuances involved in that process.
The Why:
A common (and fair) question is why a diagnostic cast is even needed for surgical guide design? A CBCT provides extensive anatomical information and the latest CBCT units can create impressive 3D renderings of the patient’s anatomy. Can a surgical guide not be created from that information? The short answer is unfortunately, no. While CBCT imaging has advanced substantially, the accuracy of the 3D renderings is still not fine enough for the millimeter precision that is needed for implant surgery. That combined with the fact that one can usually manipulate the threshold of the 3D renderings to adjust the thickness/density of the 3D images creates way too many variables for a consistent and accurate guided solution. Therefore, for now, we are still to rely on the diagnostic cast and the integral role it has in the fit and the accuracy of the surgical guide.
The Accuracy:
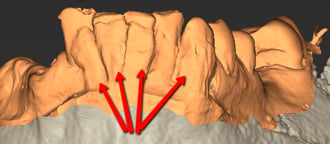
It is obvious that an accurate diagnostic cast will lead to a well-fitting surgical guide. However, it is less obvious how a well-fitting surgical guide can still lead to an inaccurate implant placement. That is because the accuracy of the diagnostic cast is only half of the equation. The other half is the merge between the diagnostic cast and the CBCT itself. The combination of these two pieces of information has many names: merge, overlay, superimposition, registration, etc. Essentially the process involves superimposing the two images and inspecting for discrepancies to ensure the diagnostic cast is accurate before proceeding to surgical guide design. The registration plays a crucial role in verifying the diagnostic cast is true to the patient’s existing anatomy and any discrepancy between the anatomy on the CBCT vs the anatomy on the diagnostic cast lets the designer know that a new impression needs to be taken. Unless the CBCT needs calibration, the inaccuracies of the registration generally arise from the diagnostic cast. However, that is not to say that lack of calibration is the only factor that can cause discrepancy coming from the CBCT. Movement, lack of definition, and excessive scatter are all examples of CBCT concerns that negatively affect the accuracy of the registration.
The 2nd purpose of the merge between the CBCT and diagnostic cast is to ensure the accurate translation of the virtual treatment plan to the actual live surgery. The implant placement is planned on the CBCT but the surgical guide is designed on the diagnostic cast. The merge is the bridge between these two pieces of information that ensures that where the implant has been planned in the CBCT will be where the physical implant will be delivered during live surgery via the surgical guide. If an accurate diagnostic cast is submitted but the merge is off during the design process, the result is the clinician receiving a surgical guide that fits beautifully but the implant position is completely off. This is where the value of an experienced designer cannot be understated. While software has advanced tools to provide impressive assisted merging, it is still not a perfect science. Scatter, distortion, and partial scans are examples of factors that can interfere with the software’s ability to accurately merge. This is where the experienced designer can either correct the merge or make the judgement call to acquire a new diagnostic cast.
The Fit:
So, we have established that the registration determines the accuracy of the surgical guide in terms of the delivery of the osteotomies and implant. We have also established that an accurate diagnostic cast results in a well-fitting surgical guide. Now the question is which method of capture yields the most accurate diagnostic cast: intraoral scan or traditional impression? Let’s explore the pros and cons of each!
Intraoral Scans
The Pros:
- Intraoral scans are generally more comfortable for the patient as it eliminates the discomfort and gag reflex caused by impression trays and material
- Intraoral scans are more efficient. Not only are they generally faster to capture than a traditional impression, but you are also able to evaluate the image immediately rather than needing to wait for the impression material to set and then pouring it up
- They are also more consistent than traditional impressions as the computer evaluates for the accuracy of the image and warns of any missing information. This takes much of the human error out of the equation
- They are completely digital, eliminating the need for purchasing and storing material. Since they are digital, they also immediately provide a STL file ready for virtual planning and design
The Cons:
- Intraoral scans can be a significant financial investment
- There is a learning curve for the office staff and may be slower to acquire than traditional impressions at first (technique sensitive)
- The software is not perfect. An experienced eye is still required to identify if sufficient information was captured for an accurate digital impression
- Requires periodic maintenance and re-calibration. Intraoral scans could also be distorted if these periodic maintenances are not being done
Traditional Impressions
The Pros:
- All dental assistants are already familiar with this procedure, therefore, it is easy to integrate (we have found that a well-taken alginate impression poured up within 10 minutes is just as accurate as a PVS for surgical guide design, so the more expensive and difficult method is not necessary!)
- Most offices are already equipped to take traditional impressions so additional investment is not needed to capture a diagnostic cast
The Cons:
- The consistency and accuracy are highly dependent on the office staff taking the impression. Even then, the best dental assistants are still humans and can make mistakes
- An impression yields a physical diagnostic cast but obviously virtual planning requires the diagnostic cast to be in a digital STL format. Now the clinician must find a solution to digitize the diagnostic cast
- Most patients find traditional impressions quite uncomfortable and patients with sensitive gag reflexes make acquisition quite challenging
- The process is generally lengthier as the impression must be taken, poured up, separated, and sometimes trimmed
- The inconvenience of having to ship these models and the risks of damage during transportation
As you can see, both options have the potential to yield an equally accurate result. However, from our experience, intraoral scans have proven to be superior due to their consistency and efficiency. For a clinician who has not yet incorporated intraoral scanners into their practice, the following options are available to digitize a physical diagnostic cast:
- Some CBCT units (such as the Vatech Green 2 and Carestream) come with a special module that allows you to capture the diagnostic cast in the CBCT and convert the image to a STL format. Please note that this is only a viable option for machines that have this functionality. Taking a general CBCT scan and trying to convert the 3D rendering to a STL creates the same inaccuracies and problems as why we cannot design a guide form a CBCT in the first place
- There are many desk-top optical scanners in the market that allow you to scan a physical diagnostic cast to produce a STL
- You can ship the diagnostic cast to a local lab or Implant Concierge to have the model digitized for you
Evaluating a Diagnostic Cast
Ultimately, the technician designing the surgical guide will be the final evaluator of the quality of the diagnostic cast. That may be your local lab, a 3rd party company such as Implant Concierge, or even yourself as the clinician should you choose to take on that responsibility! Even if you are planning to outsource the surgical guide design, it is beneficial to be familiar with common issues to look out for when evaluating a diagnostic cast. This will help avoid secondary appointments for new impressions and will save both the office and the patient time and money. Here are some common problems we encounter at Implant Concierge:
Intraoral Scans
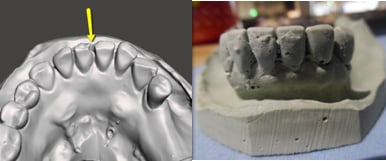
- Missing data:
- Quadrant Scans: While this is not inherently a problem, please keep in mind that a quadrant scan (vs a full arch scan) will only allow the accurate design of a quadrant surgical guide. This causes potential stability issues due to the lack of cross-arch stability
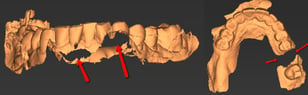
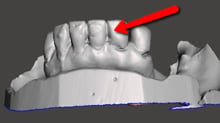
- Triangulation/stitching:
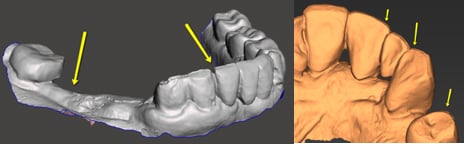
Problems with the stitching or triangulation will need to be addressed to the intraoral scan manufacturer for calibration and troubleshooting. From our understanding, stitching can also be caused by the quick transition from one surface to the other by the technician. Missing some information in that quick transition causes the software to “stitch” one surface to the other causing that line that is commonly seen in the occlusal/incisal edges.
Traditional Impression
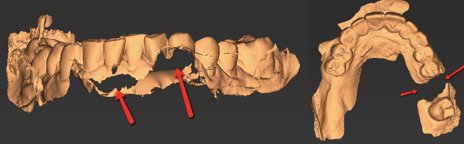
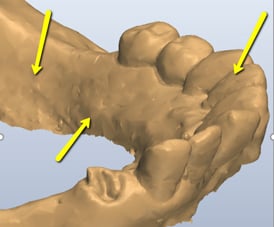
- Bubbles/Chips/Cracks:
The concavities that result from bubbles, chips, etc. will be filled in with resin during the guide design step. Since these voids are not actually present in the patient’s dentition, the resulting artifacts on the surgical guide will prevent the surgical guide from seating properly or at all.
- Drag/Excess Material:
The protrusions created by drag or excess material on the diagnostic cast can result in a loose-fitting surgical guide. If minor, sometimes this can be negligible but when the artifacts are extensive the guide can be loose to the point of rocking.
In conclusion, there are many variables to consider when taking an impression with a guided solution in mind. Those variables will be dependent on the method of capture, physical vs digital. Regardless of the route chosen, the accuracy and registration of the diagnostic cast will be the ultimate determining factor of the success of the surgical guide. At Implant Concierge, we have several steps of quality control checks to ensure stable and accurate surgical guides. Implant Concierge is here to help support clinicians in education, guided surgery evaluation, and to serve as a comprehensive digital dentistry concierge service to help offices integrate and succeed with guided surgery. Please do not hesitate to reach out to us at any time for more information on this topic or anything related to digital implant dentistry!